|
Women's health physios do not just teach kegels! And this list is not exhaustive. These are just some of the most common problems I see in my clinic each week.
You can get a referral via your GP for NHS physio or there is a large private network of physios in the UK, which accept self referral. You can book an appointment with our clinic by clicking here
0 Comments
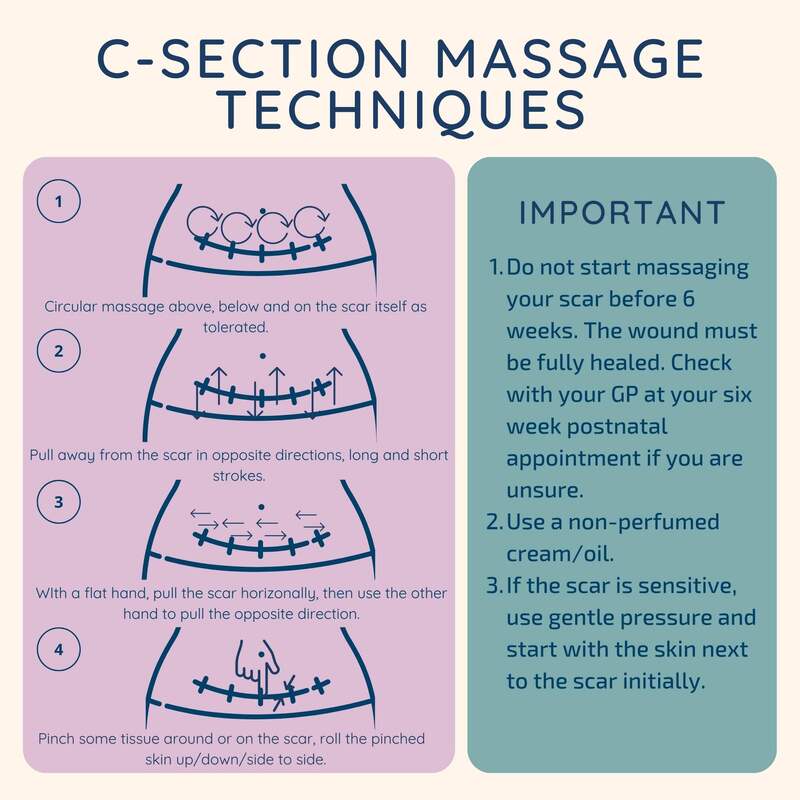
Just a few minutes of massage a day can make all the difference to your scar healing.
Massage helps to: Break down unnecessary scar adhesions Reduce scar sensitivity Improve the mobility of the skin Reduce scar related pain These are simple techniques that can be easily implemented by someone who has a c-section scar. If you do not think you scar is improving or you are finding it painful, book in to see a physiotherapist. I was prompted to share this post because I've had a really nasty bout of coccyx pain recently. However - I've utilised some of these strategies and it's now resolved!
1. Offloading the tailbone is important during sitting. You can buy lots of different ring cushions on amazon but I find the blow up travel neck pillows have worked a treat for me! 2. The pelvic floor can often aggravate or contribute to tailbone pain so pelvic floor stretches can be very helpful in relieving symptoms. 3. Manual therapy doesn't work for everyone but when it does it's great! I then give patients a way of self treating at home. 4. You can try heat or ice, whichever gives relief. I definitely prefer warmth but see what works for you. 5. The coccyx is part of the spine so low back problems can also contribute to tailbone pain. Therefore it is important the spine as a whole is moving freely. Incorporate some spinal mobility exercises into your daily exercise programme. 6. Make sure you are not sitting in a slouched position because this loads the coccyx and can irritate it further. Make sure you're are sitting on your sitting bones (the bony bits in your bottom), not your tailbone!
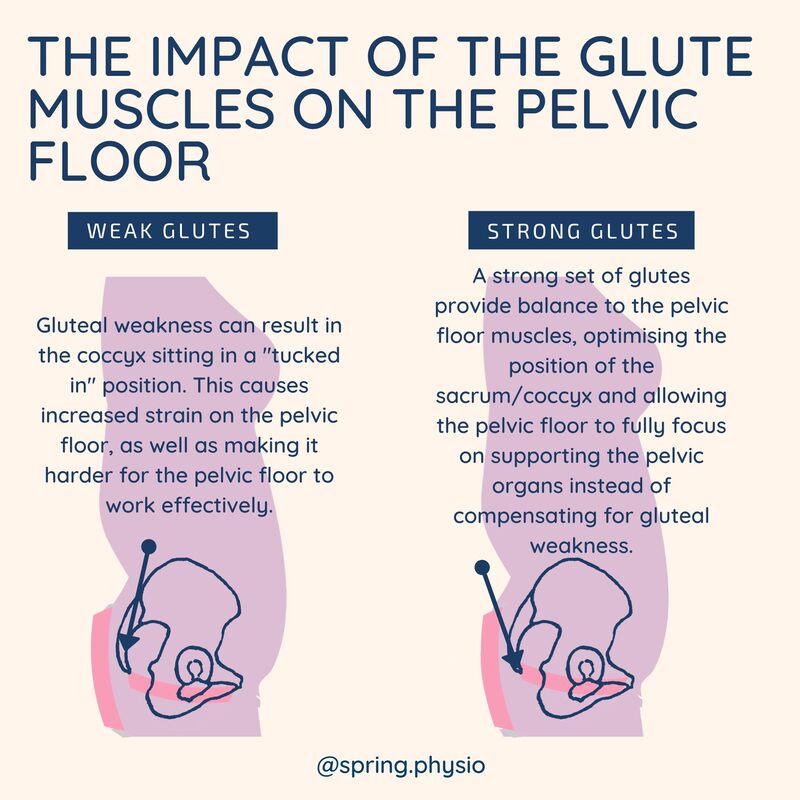
If your pelvic floor rehab doesn't include some kind of glute strengthening, now is the time to get started! Strong glutes allow your pelvic floor to focus on what it's best at - supporting your pelvic organs and keeping you continent!
I was delighted to produce this infographic for the POGP journal to support Christien Bird's presentation at the POGP conference last year.
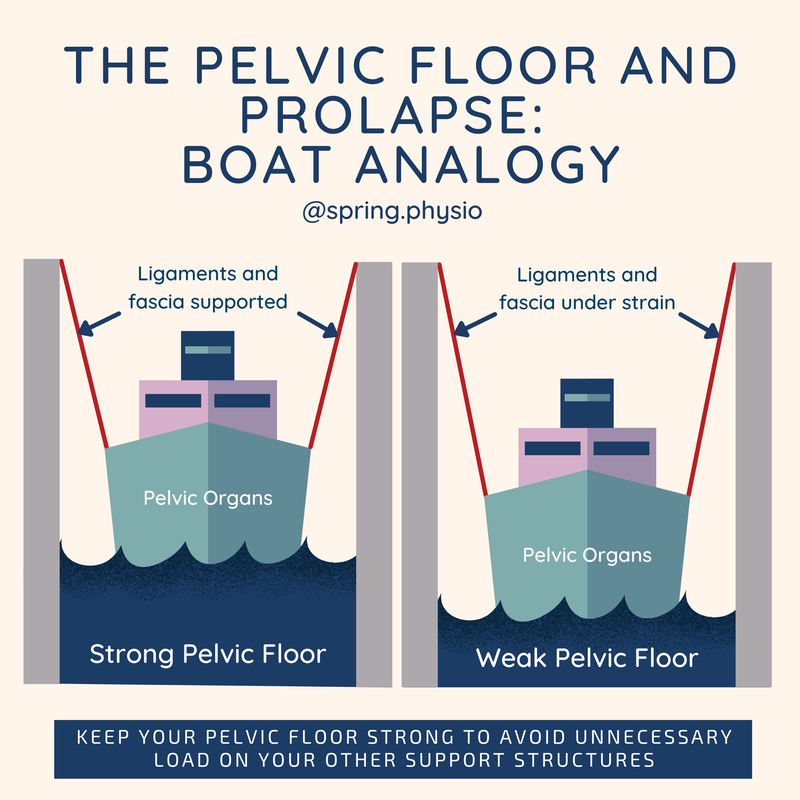
The presentation by Christien covered many different aspects of menopause management but the three key elements that all women need are good sleep, good diet and regular exercise. There is lots of confusing information out there, especially about diet in menopause. But the take home from the presentation was this: Manage your blood sugar levels. The easiest way to do this is through eating a combination of protein and complex carbohydrates. There is a tendency for women to "go to the mat" in the peri/post menopausal years. Whilst there are lots of benefits to doing lower impact mat based exercise, the benefits or doing a mixture of exercise types (including resistance and higher impact) are incredibly important for optimising muscle mass and bone density. Variety is key! The boat in the dock theory (Delancey et al) is a way of illustrating the relationship between the pelvic organs (the boat) pelvic floor (sea), ligaments (ropes) and prolapse.
A weak pelvic floor doesn't cause a prolapse. But over time not having that support puts more strain on the other support systems, which in turn can cause more stretching or damage to the support system. The best approach is to always maintain a strong pelvic floor. If you then stretch or injure any of the connective tissue supports (eg through pregnancy or childbirth), you've still got some solid muscular support. If you've already gott a prolapse and haven't had any pelvic floor strengthening, hopefully you can see from this image why it's so important! There is little conclusive evidence on the best method of rehabilitating a diastasis. The aim of this infographic was to provide a bite size reference for best practice approach, based on the evidence that is available for managing the condition. It also aims to raise awareness ofthose less familiar with treating diastasis, to give them an overall view on management. The take home message is that there is no one size fits all method and that each patient will
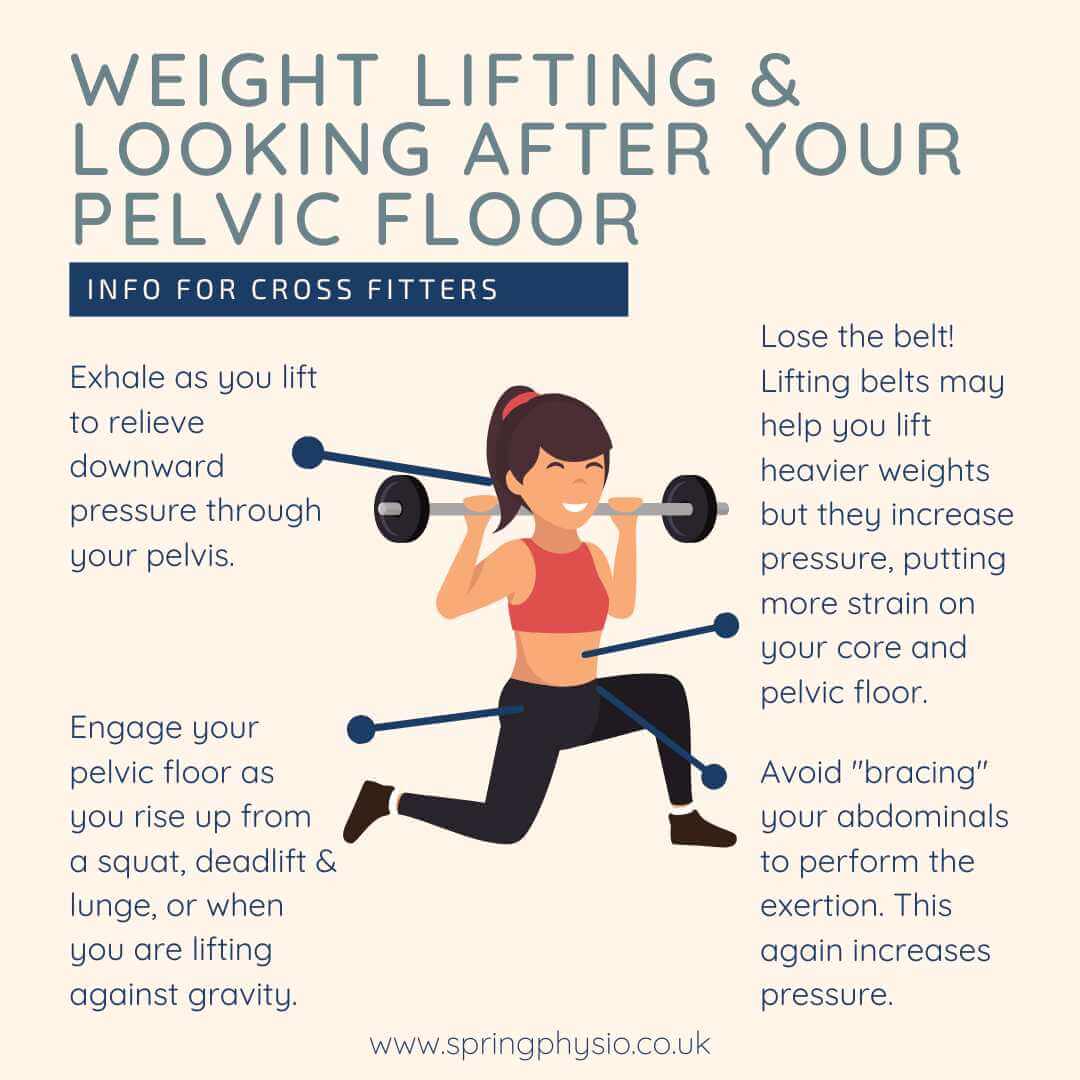
need an individualised approach. The poster highlights the need to focus on tension of the linea alba, rather than gap size. This is supported by literature evidence that inter recti distance can actually increase with TVA contraction (Lee and Hodges, 2015 and Theodorsen et al, 2019). The basis of rehab is therefore focussed on tension rather than whether the gap physically decreases during the exercise. Assessing functional response to exercise on an individual basis can potentially give them more freedom to return to the things they love. The functional ability will vary person to person, even if the diastasis presents similarly to another in size or tension.The focus should be on whether clients can create tension across the linea alba during the task, rather than relying on gap size. When functional activities are not yet appropriate, rehabilitation can be goal specific and modifications set. Further research is needed to identify which rehab protocol of strengthening provides the best results, in order that we can confidently offer our patients the best possible treatment outcome that is evidence based. Leaking in cross fitters is common... and often considered a normal side effect of lifting heavy weights. But guess what, it doesn't have to be. You can cross fit/lift heavy weights and not leak! A women's health physiotherapist can make sure your pelvic rehab is functional and will meet the demands of your lifting regime. Here are some top tips for those that want to lift weights but also ensure they are protecting their pelvic floor.
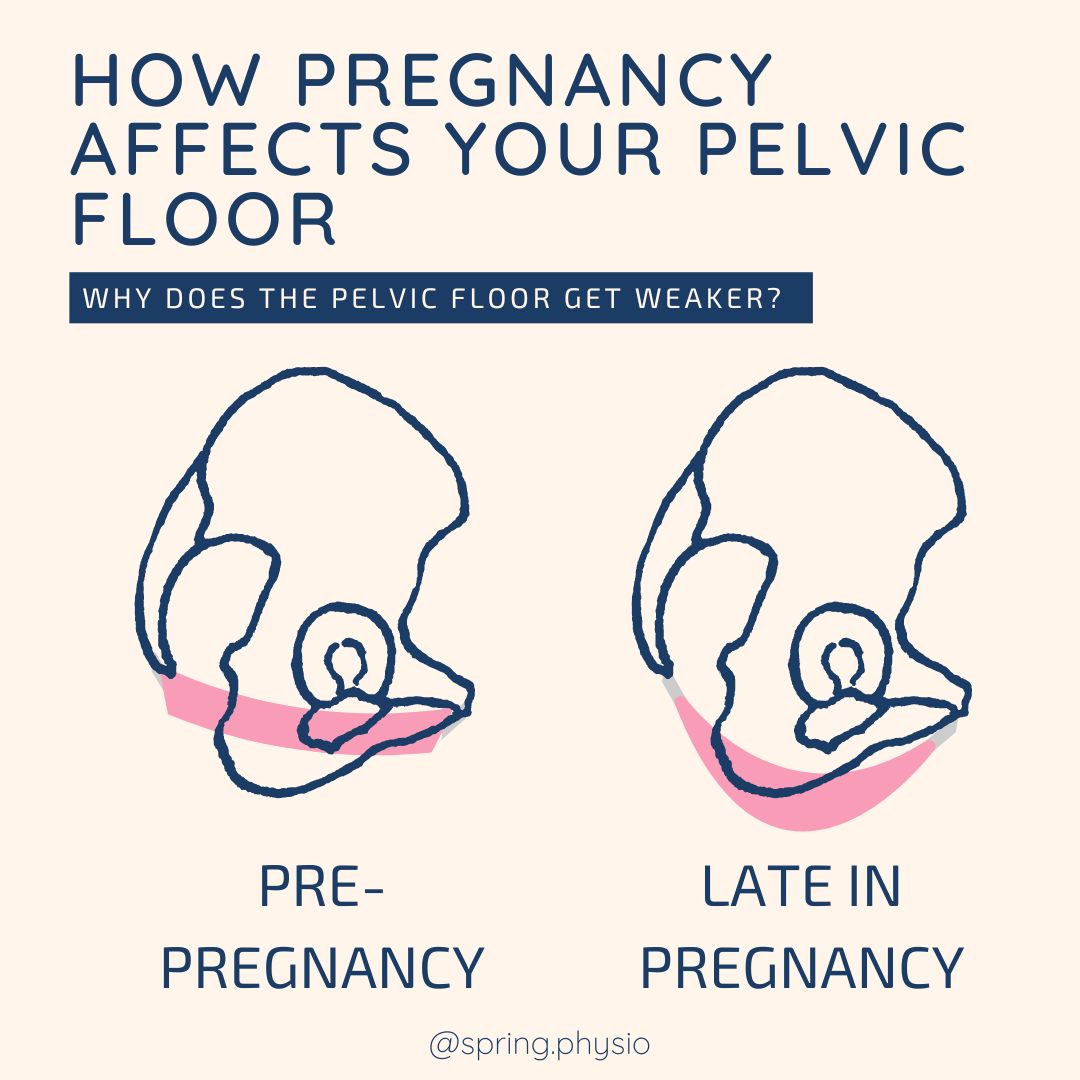
1. Exhale during the exertion. This reduces the pressure going through your pelvis during the lift. 2. Belts increase pressure, which is exactly what we want to avoid to reduce urinary leakage or other pelvic floor symptoms. You may feel you can lift heavier with a belt on, but long term you pelvic floor won't thank you for it. 4. Engage your pelvic floor as your exhale through the exertion. This gives extra support and helps to manage any pressure. Make sure you let go of your pelvic floor at the end of the exertion. 5. Focus on pelvic floor engagement rather than bracing your abdominals during the lift. Engaging your abdominals alone actually increases the amount of pressure during the lift. During pregnancy, the additional load of the baby and the uterus cause changes to the bladder, urethra and the pelvic floor. This weight creates a lot of additional work for the pelvic floor and as a result the muscles can become weaker. The hormonal changes occurring in pregnancy soften the ligaments and muscles around the pelvis to allow stretching for delivery, but again this makes it much harder for the pelvic floor to contract well. By the end of pregnancy your pelvic floor can lack the tone and strength that was there at the start of pregnancy (especially if you haven’t been doing any pelvic floor floor work in pregnancy!), making symptoms related to pelvic floor weakness very common. It is because of these changes that EVERY woman should do pelvic floor rehab after a baby, regardless of how you delivered or whether you have symptoms.
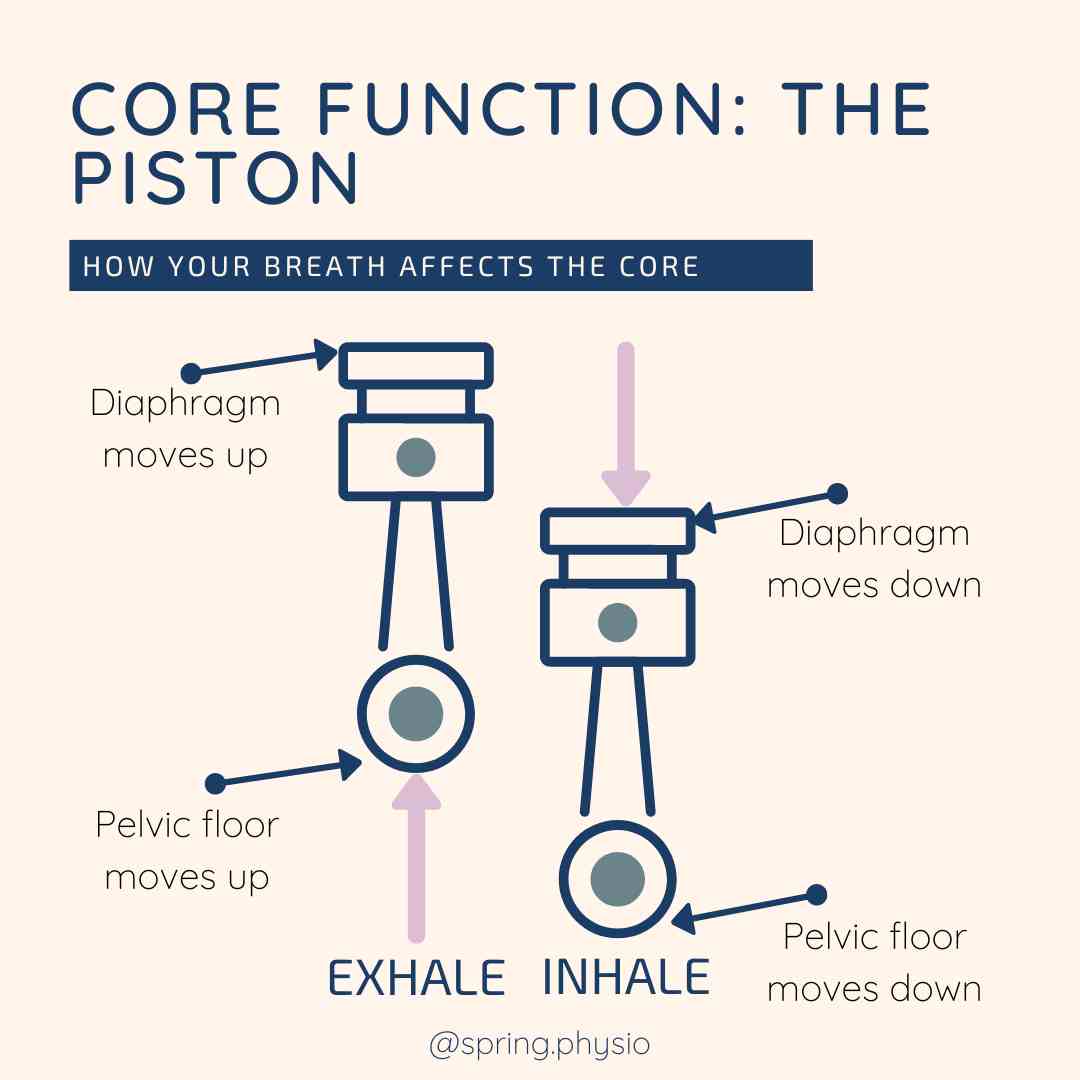
I believe the piston analogy originally comes from Julie Wiebe. It is a great analogy to help patients understand how their core relates to their breath. As you exhale, your diaphragm and pelvic floor are naturally shortening - the piston is moving up. Performing a pelvic floor and core contraction on the exhale makes it much easier to engage the muscles, because you are joining in with the natural movement of the core. When you inhale, your diaphragm and pelvic floor move down to help make space for the lungs tor fill with air - the piston is moving down. Trying to contract the pelvic floor on inhale is much more difficult, because it goes against the natural direction that the muscles are moving in. For this reason core exercises are performed on the exhale.
|
AuthorClaire is a women's health and sports Physiotherapist. She is the owner of Spring Physio and is based in East Sussex. Archives
April 2024
Categories
All
|





 RSS Feed
RSS Feed