|
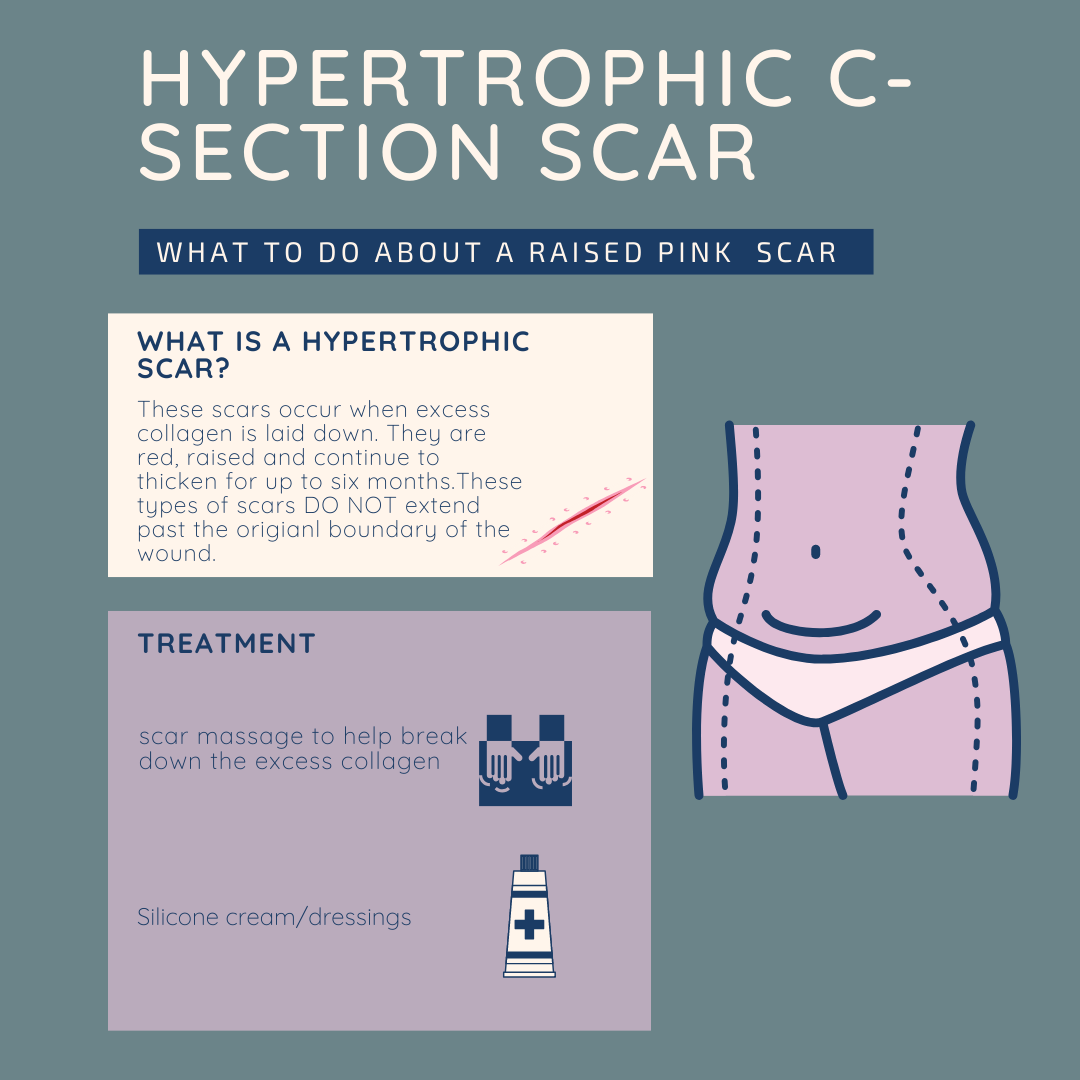
.Pink and raised scars are pretty common... and people tend not to realise that there is something that can be done about them! Both these treatments can be carried out at home once your physiotherapist has explained how to implement them.
The NICE guidelines recognised silicone as a good treatment option for hypertrophic scars. Dressings are available on prescription on can be purchased online. My favourite silicone option is Kelo-cote scar gel. There are other in clinic interventions such as laser treatment, but massage and silicone is a great place to start.
0 Comments
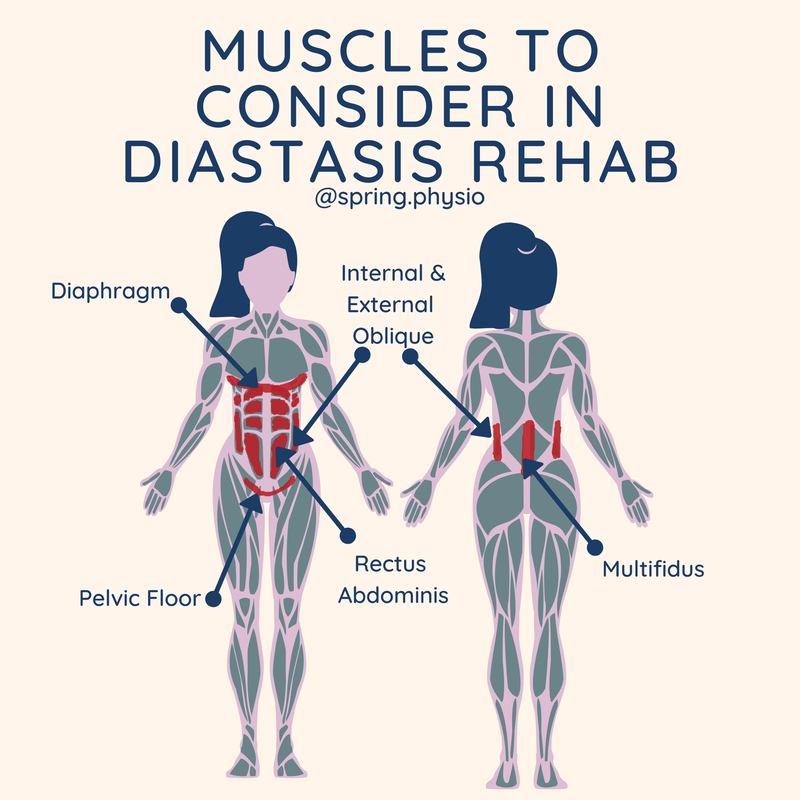
Diastasis is a whole body issue. So much focus can be placed on TVA that the rest of the core cylinder can be forgotten. Our core is not designed to work as individual muscles, but as a "cylinder" of support comprising of the diaphragm, TVA (deep abdominals, pelvic floor and mulitifidus (deep spinal muscles). When we re rehab a diastasis, the whole core has to be involved.
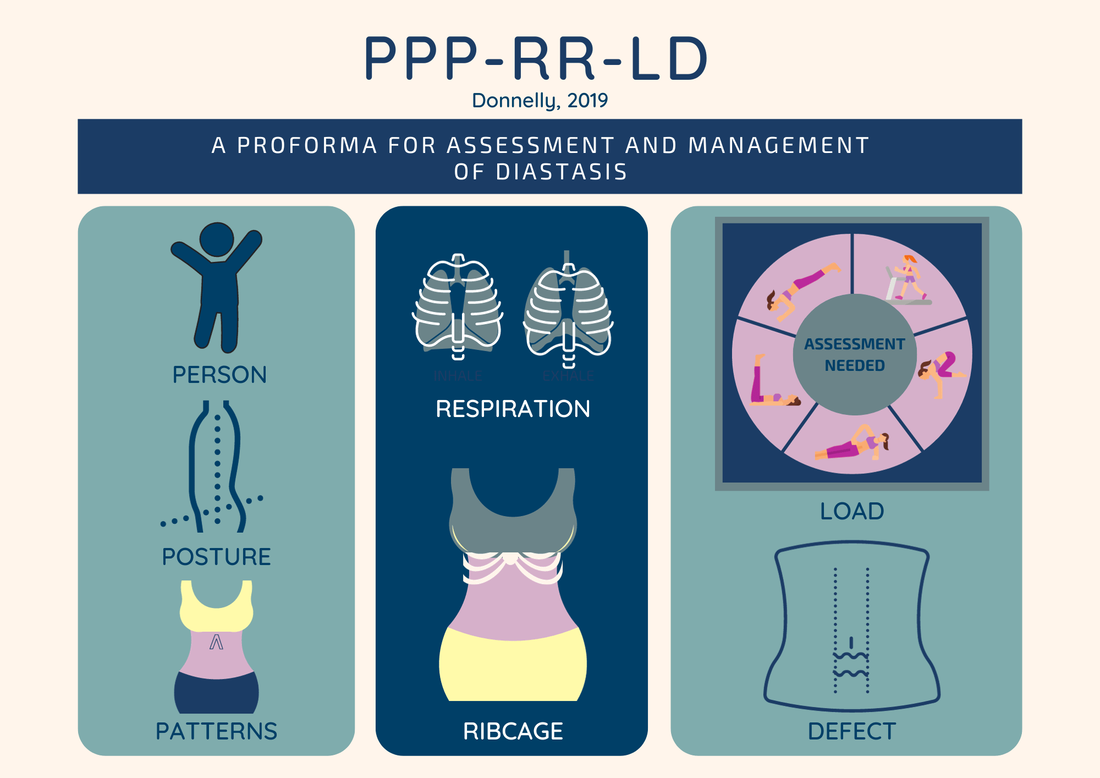
If any non-core muscle is restricting any element of the cylinder, it is also going to have an affect on the deep abdominals. For example, if your obliques are tight and your diaphragm is not moving freely as you breathe, one element of the core cylinder is restricted. When you try and do your core exercises, the lack of diaphragm engagement is going to make the whole core less well engaged, reducing the effectiveness of the core exercise to heal the diastasis. So if you've tried a load of core exercises/pilates and you haven't seen the results your looking for, consider seeing your local woman's health physio for a thorough assessment. This acronym was developed by Grainne Donnelly, as a proforma for assessing and managing diastasis. The acronym covers the key areas of assessment:
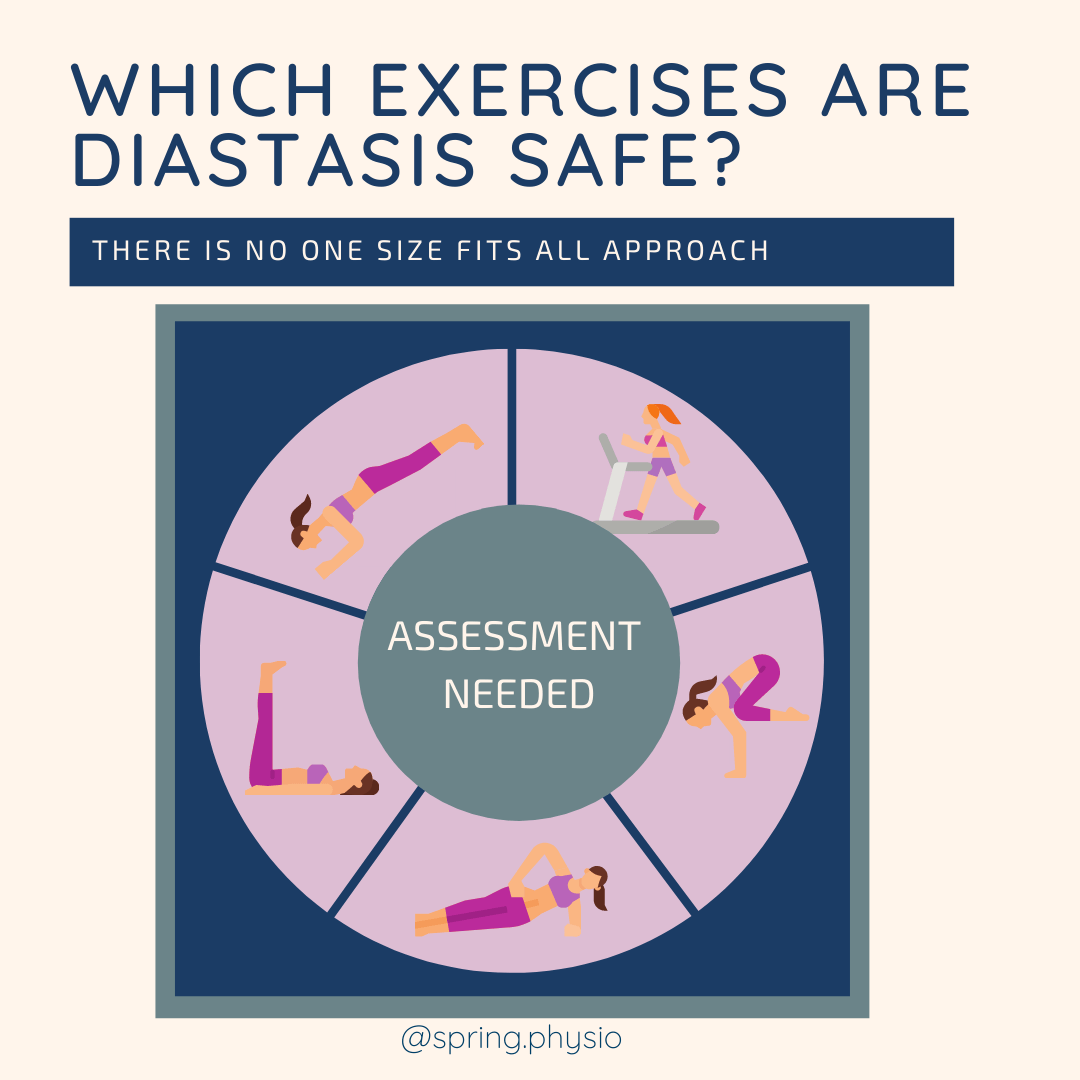
1.Person - understanding who you are treating and their personal journey 2.Posture 3.Patterns (of movement - eg. abdominal bracing) 4.Respiration- (is breathing optimal for core recovery?) 5.Ribcage (assess compensatory strategies, flaring, asymmetry, infrasternal angle) 6.Load (assessing the abdominal wall with different types of load) 7.Defect (Are there any other defects? eg hernia) Assessing each of these areas will help you identify factors that could be contributing to an ongoing diastasis. Addressing any compensatory strategies, suboptimal breathing, altered movement patterns and postural changes will ensure your rehab is bespoke and address the function of the abdominal wall, not just the gap. This is such a great road map for how to approach diastasis holistically and FUNCTIONALLY. If you treat diastasis go read it!!! You can read the full article here: "Donnelly G. (2019) Diastasis rectus abdominis: physiotherapy management. Journal of Pelvic, Obstetric and Gynaecological Physiotherapy 124 (Spring), 15–19. You may have been told that you shouldn't plank, run or do various sits up with a diastasis. Spend a little time on google and you will find lots of diastasis "safe" and "unsafe" exercises.
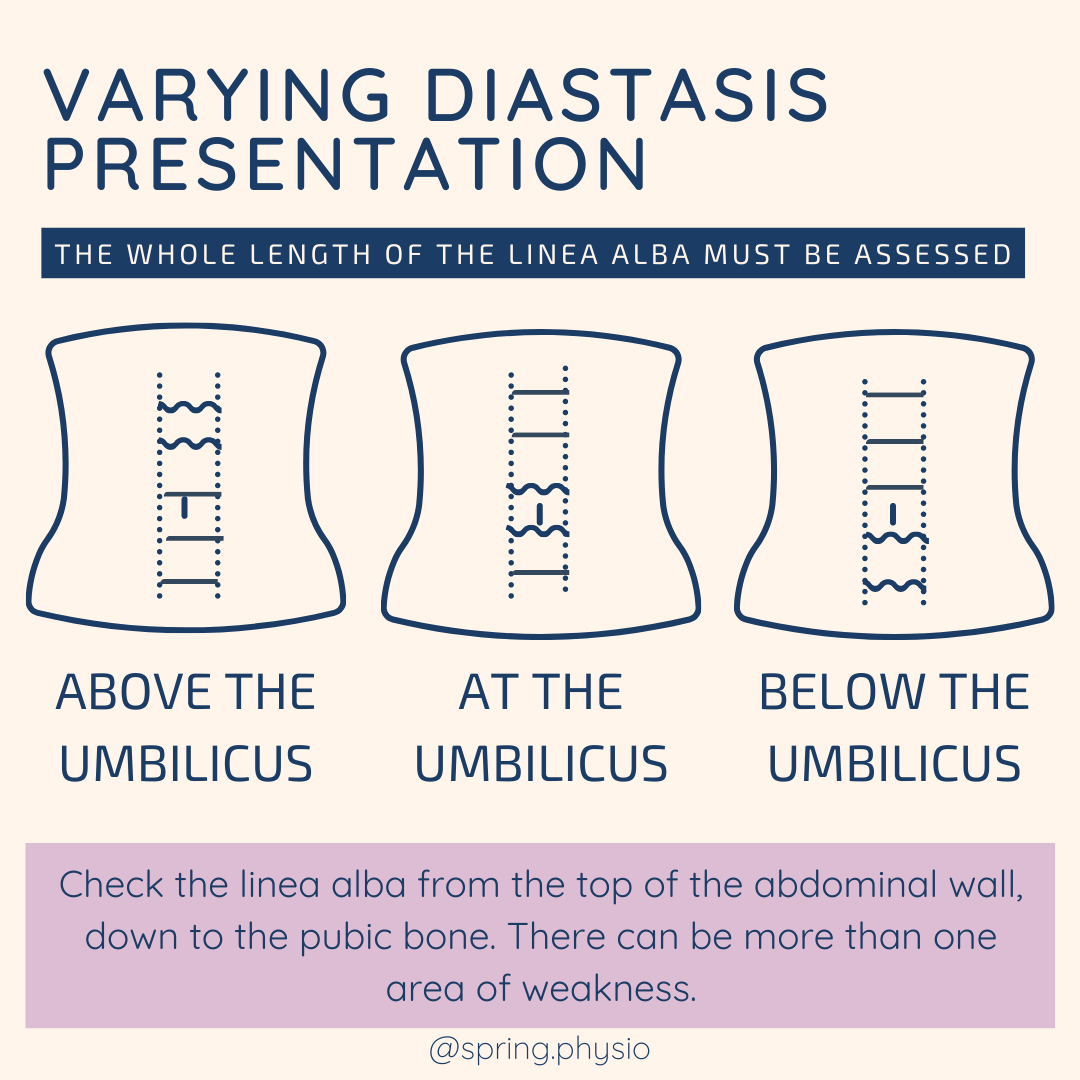
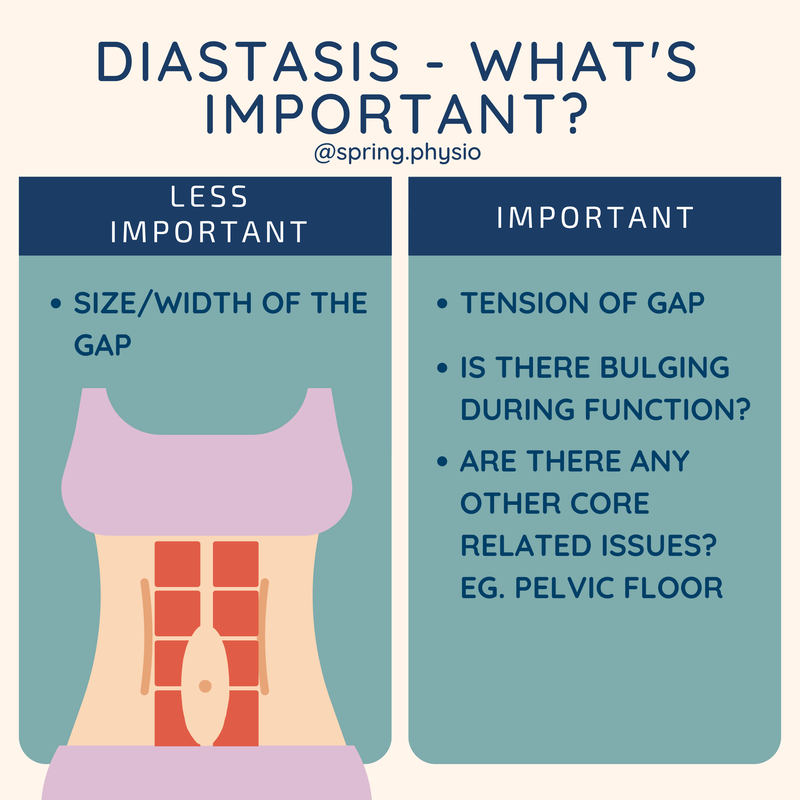
The fact is that everyone is different, because diastasis isn’t a blanket diagnosis and functional ability varies person to person. One person may dome when they front plank, but be fine when they do a sit up; some one else might be the opposite. It's so important to get a proper assessment of the linea alba and core muscle activation doing functional movements, otherwise you may be missing out on that high level yoga class unnecessarily. A physiotherapist can assess the size and tension of a diastasis gap, but also the functional movements or exercises that doming. Once this has been established, a suitable strengthening programme can be given to regain strength and control to prevent doming in those specific movement planes. Diastasis refers to a separation of the rectus abdominis muscles across the linea alba. Diastasis occurs naturally in pregnancy, but can continue in some women in the postnatal period. The presentation of diastasis can vary, so thorough examination is important. Here are some of the factors that can vary from person to person.
1. Width and Depth It is important to assess both the width and the "softness" of the gap on palpation. An ongoing gap with firm tension shows that there is good abdominal strength, and often rehab is not required. A gap with soft tension tends to pose more issues with doming and will require rehab. 2.Location The separation might be more pronounced at different points along the midline of the abdomen (see above image). The gap is commonly largest around the belly button area, but can occur higher or lower. 3.Associated Symptoms Often diastasis goes hand in hand with other core related symptoms such as incontinence and back pain. Understanding these variations can help healthcare professionals assess and guide appropriate treatment, which may include exercises and physiotherapy. It can be tempting to think you might be able to self treat a pelvic floor problem. Add in a few kegels to your day and all will be sorted right?
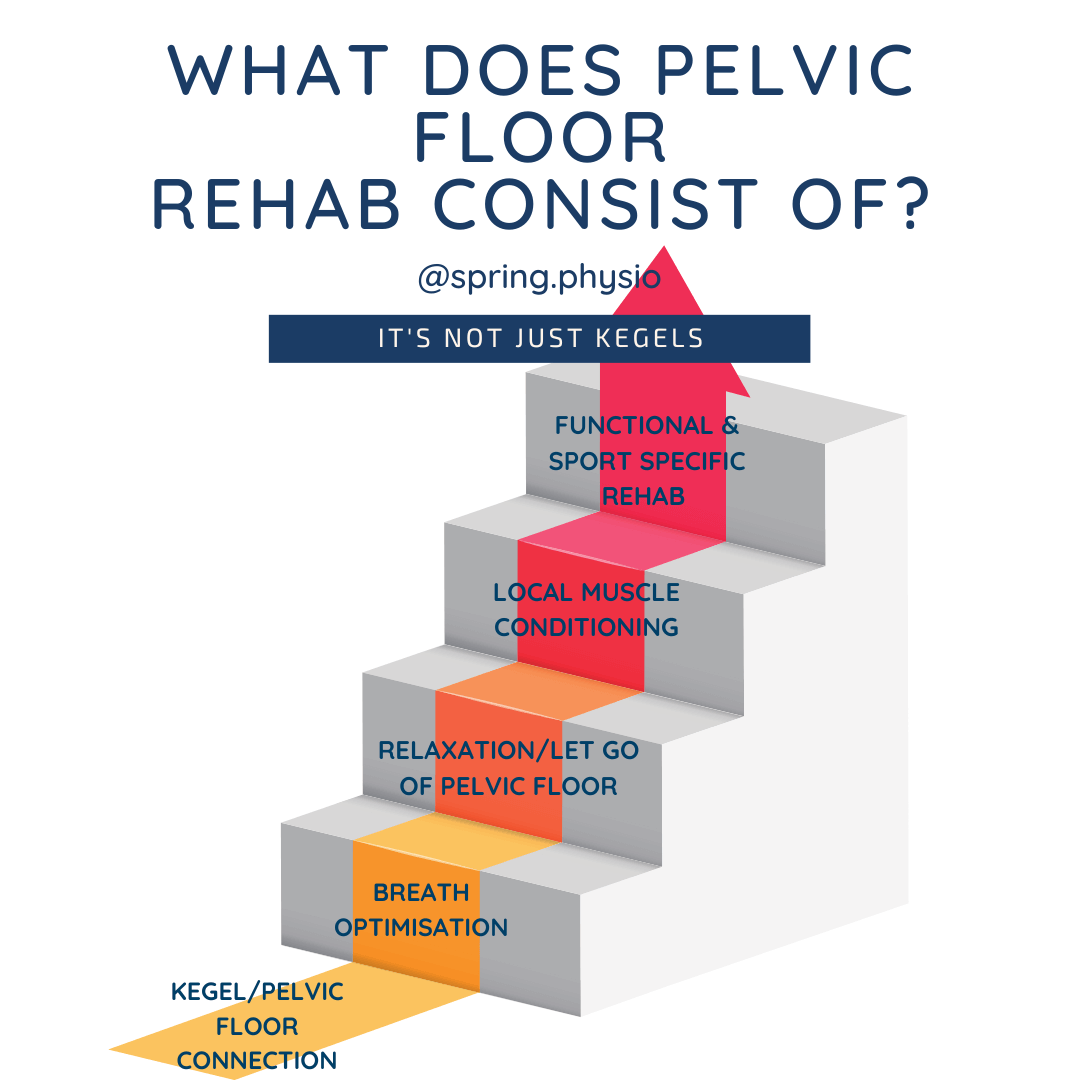
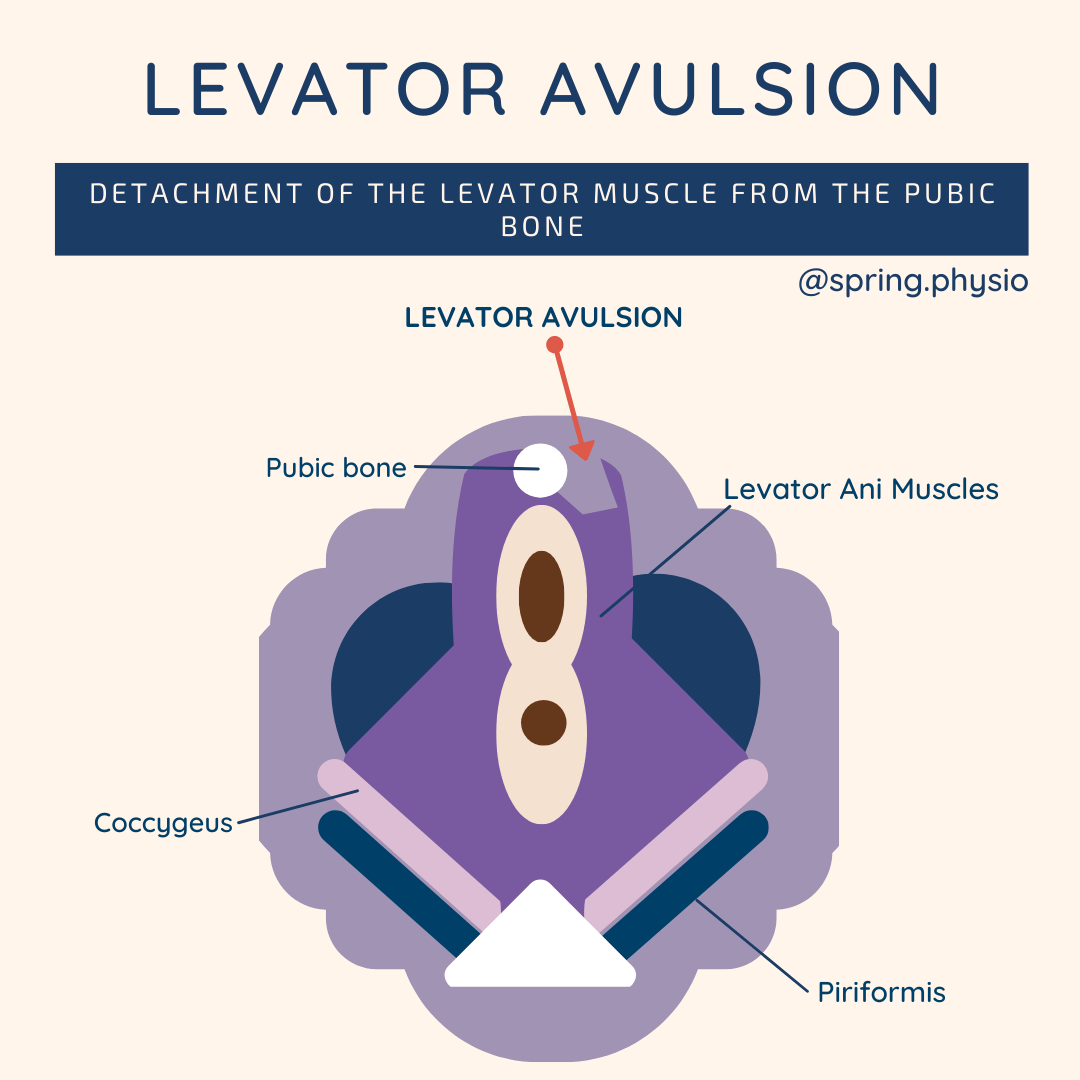
- Not all pelvic floor problems are solved by kegels (doing pelvic floor contraction work), for example: certain pain conditions or tight/hypertonic pelvic floors - If a contraction is appropriate but your technique is wrong, it won't be effective. - Part of pelvic floor rehab is starting at an appropriate level and then progressing appropriately. If you start at the wrong level or don't progress at the right time you may find you don't improve. - It's imperative to make your pelvic floor rehab activity/sport specific to ensure you achieve full resolution of your symptoms during higher lev.el activity Conclusion? Get your GP to refer you to your local NHS physio service or contact your local private pelvic floor physio for a full assessment and treatment. A levator avulsion is where part of the pelvic floor muscles are pulled off the pubic bone. This can affect between 10-35% of women following their first delivery.
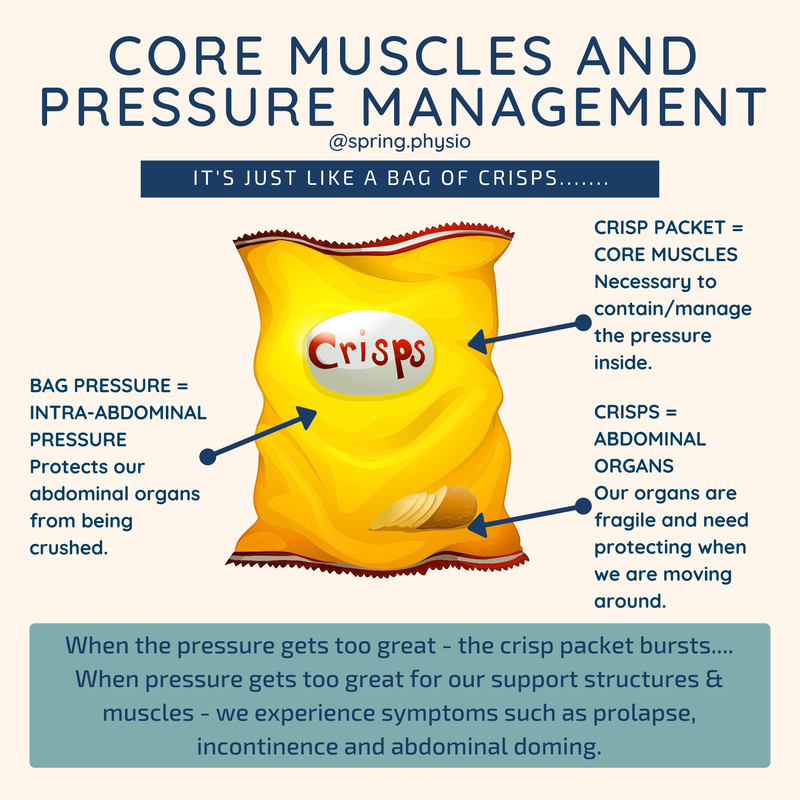
The loss of this support can make your pelvic floor weaker, enlarge the opening of the vagina and increase the likelihood of prolapse. A levator injury is not repaired, but if you have been diagnosed with one it makes it even more important to strengthen the intact pelvic muscles - to provide as much support as possible to the pelvic organs. Levator injuries are often not diagnosed immediately but may be picked up by your physiotherapist or gynaecologist during a pelvic examination. I use this analogy all the time in clinic to help patients understand the importance of managing their pressure to help improve core/pelvic floor symptoms. Pelvic floor symptoms such as prolapse and incontinence tend to be worse in high pressure situations, when the crisp packet (the core) is overwhelmed.
Breathing is an easy way to reduce pressure. If we exhale rather than hold our breath on exertion, there is less pressure being held "in the crisp packet" that has to be managed by the core muscles. If you have symptoms on a particular activity - such as running/HIIT or cross fit, see your local women's health physio. They will be able to modify your activity to better manage the pressure you are producing with that activity. There seems to be concern amongst those who have a diastasis that gap size determines whether they have recovered . Whilst gap width is something we assess in clinic, there are more important aspects of diastasis that need to be assessed:
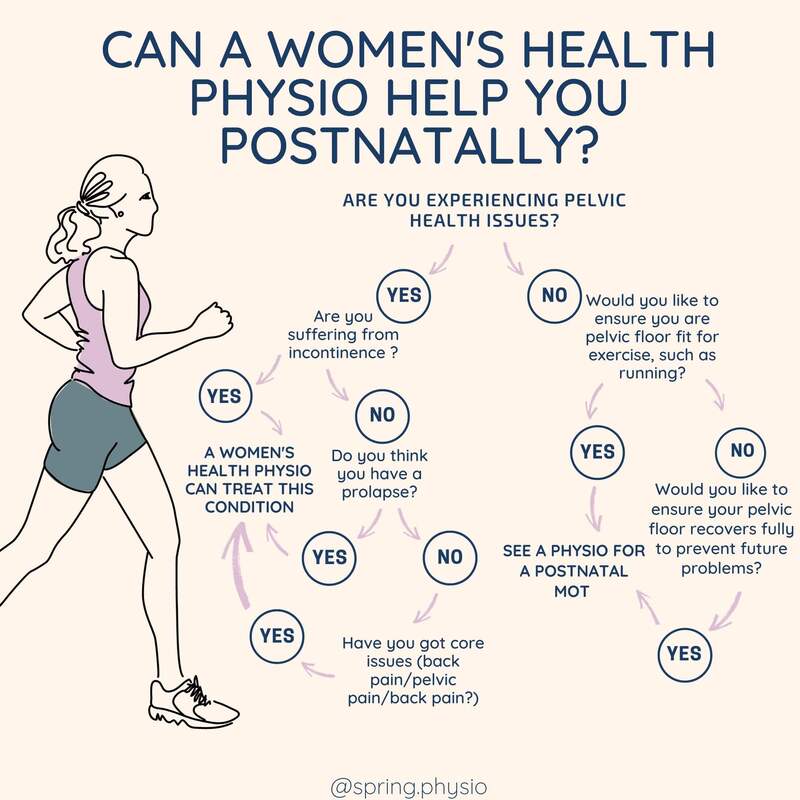
1) How much tension you can generate across the gap during load? For example: during an abdominal curl up. If you put your finger on the gap whilst performing a curl and you feel it’s tense/firm, that’s a good sign 👍. It shows the abdominals are engaging ok. If it is very soft, some more rehab is needed. 2)Is there doming/bulging on functional activities? I have seen women with a very small gap who have significant doming during high level activities, and those who have a bigger gap that don’t dome at all. That’s why assessment is so important. You shouldn’t be frightened to exercise - a Physio can give you very specific guidance about what activities you can do (and I bet they say you can do more than you expect). The key is modification. 3) How is the rest of the core performing? It's important not to just look at one element of core function because every woman should be treated holistically. If someone has a pelvic floor issue as well as diastasis, this should be assessed too. It is possible to kill two birds with one stone when setting up a rehab programme; two core issues can be treated together. Are you unsure where to go for help postnatally? Are you experiencing symptoms but are unsure what treatment is available? A women's health physio is ready to help you. In most cases, conservative physiotherapy management is effective in dealing with common issues such as diastasis, incontinence, pelvic pain/back pain and prolapse. Use this flow chart to see how pelvic floor therapy can help you!
|
AuthorClaire is a women's health and sports Physiotherapist. She is the owner of Spring Physio and is based in East Sussex. Archives
April 2024
Categories
All
|

 RSS Feed
RSS Feed